When I was young I wanted to work with what I thought of as the poor and underserved. Over the course of my career, I’ve worked in four types of facilities: mental health facilities, homeless shelters, prisons, and detention facilities. They all share similarities. I was excited when my first job out of college was at St. Elizabeths Hospital in Washington, DC working on a unit for those who had a mental illness and “no fixed address” which was the systems euphemism for homeless.
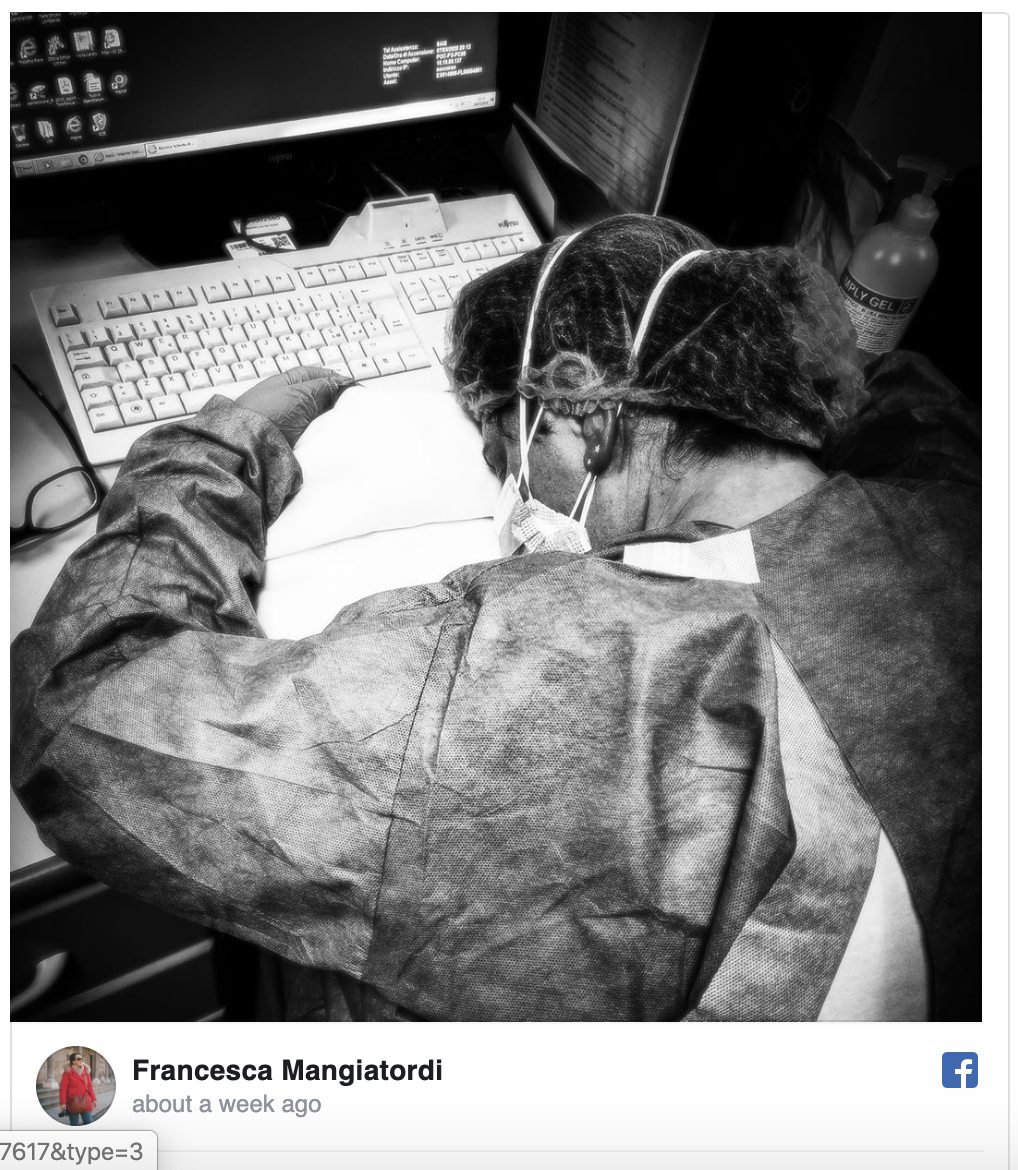
The unit and the hospital was largely still as Ervin Goffman described it in Asylums. While the harshest of treatments had long ago ended they were still given donated clothing or hospital purchased clothing to patients and generally not returning their clothing. The food was dismal and best. There were times when the food was so limited that patients checked out against medical advise. The conditions for staff were also not what most would expect. Nursing was chronically understaffed and depended heavily on per diem nurses. There were long periods when nurses were forced to work overtime that could be an additional shift or even an additional day or more. Anyone who thinks forcing people to work multiple shifts of overtime a week improves quality of care or compassion is delusional. I don’t know if any of us complained about or filed protest through official channels or even thought to do so. I do know that many of us donated our used clothing and brought food that we cooked and shared with patients.
I volunteered in shelters and tried to understand what could be done to change a society that allowed so many people experiencing homelessness to go without the medical, mental health, and social services care they needed. There was only one answer, we are still a puritanical society that sees the plight of those experiencing homelessness as just punishment for sloth. I suspect many believe mental illness is a myth and so when the mentally were deinstitutionalized under President Regan with the promise of outpatient care that never materialized people complained and shouted at the wind, but we still don’t have adequate outpatient care?
Mental illness is nothing to be ashamed of but stigma and bias shame us all. – Bill Clinton
After three years I ask for and received a transfer to the Federal Bureau of Prisons in Tucson, AZ leaving the care of one group of people held against their will to care for another. FCI Tucson was in many ways a model facility. It was clean, efficiently run, had fully staffed medical and dental clinics, lab, psychology, and pharmacy. The food was good and most of the staff ate the same food as the “inmates”. Those that worked in UNICOR were paid and a commissary was available to purchase things that were not provided. In fact, many of those who were there for illegal reentry into the U.S. would send some of their money home. It wasn’t what I had in mind when I thought of working with the poor and underserved, but there were many similarities to large psychiatric facilities through the prisons seemed better funded and better staffed. We seemed to treat those in prison with more respect and compassion that either those with a mental illness or those experiencing homelessness.
I was in prison and you came to visit me … I tell you the truth, whatever you did for one of the least of these brothers of mine, you did for me.”
(Matthew 25:36, 40)
It was at FCI Tucson that I began to realize that to make big changes one had to be able to change national policy. The Federal Bureau of Prisons is not luxurious, but most of their federally run facilities comply with the American Correctional Association and National Commission on Correctional Healthcare guidelines. In fact, while I was at FCI Tucson we sought and were accredited by the Joint Commission. If one wanted to be an administrator there was a training program that had to be completed and thus there were standards. Every person working there had to complete annual training and sign off confirming they knew the rules. There will always be bad actors, but they were the exception. In my time there if I ask for anyone to be sent out to the local hospital it was not debated. It happened and generally happened quickly.
In 1997, I became the Health Services Administration at the Buffalo Federal Detention Center. Medical care was run by the Division of Immigration Health Services (DIHS). Many of the people were pending deportation after serving time in prison. When I arrived the medical clinic was still under construction. I hired a physician, two nurse practitioners, an RN, an LPN, two medical records techs, a pharmacist, and a pharmacy tech. We had a dentist and a psychologist that came in on a regular basis. Additionally, we invested in telemedicine equipment which at the time was new and gave us access to other providers. Within fifteen months of opening, we were accredited by the ACA, NCCHC, and Joint Commission. In my time there we had no deaths and provided high-quality care. My biggest complaint was the inability to get patients brought to us in a timely fashion and too often being told someone had been removed from the facility when in fact they were still there.
I became the Chief of Field Operations responsible for administrative oversight of the eleven health clinics in Immigration detention facilities (not contract facilities). I visited most of them and did a thorough review of any deaths. Most of the healthcare staff were U.S. Public Health Service officers and so most were passionate about their work and caring for those in detention. There were exceptions and some people over time became judgmental about the plight of those detained, but in my worst nightmare, the worst case I reviewed, the worst thing ever reported to me doesn’t equal what is happening today with the detained children. More importantly, if any of what is happening now was reported Immigration and DIHS would have immediately sent teams to investigate.
I left DIHS in 2001 after 9/11 when to run the command center for Secretary Thompson’s at the Department of Health and Human Services. I never returned to DIHS and was grateful as I had become increasingly concerned about what I saw as a push to limit the care provided and a move to more contract facilities and more contract staff. Physicians were feeling overworked and nurses were being asked to take on more and more of the care. While I didn’t think nurses were being asked to do anything out of their scope of practice it was a constant battle to not cross that line. I also knew I was pushing the envelope. I was told at one point, “You will do the right thing no matter the consequences.” It was not meant to be a compliment. The person was angry and my life was becoming more difficult.
In 2007, I went to work for the Administration for Children and Families (ACF) as the director of the Office of Human Services Emergency Preparedness. I worked closely with the Office of Refugee Resettlement( ORR). The reason for the visits was twofold, assess their emergency preparedness and see how they did case management. ORR was considered to have an excellent case management program that moved people from being a new refugee that didn’t speak English to being fully self-sufficient in six months. It was a huge effort that was supported by faith-based organizations. I visited a few of the facilities for unaccompanied children and I did find them depressing, but they were clean, each child had a bed with linens and blankets, age-appropriate clothing, plenty of food, medical care (which I didn’t think was at the level I would have liked), and education though it certainly was not equivalent to elementary or secondary schools in the community. There were around 40 facilities and 1600 beds. They were chronically underfunded even then. What they could do was limited by the funding. Congress and the White House knew it. In fact, the faith-based organizations that ran many of the facilities also knew about the underfunding.
This is my long way of saying I could not believe what I was hearing when the detention facilities were referred to as concentration camps and there was inadequate food, no basic sanitary supplies, inadequate medical care, and children taking care of children. The places I worked and visited were not great, but I called the people working there colleagues and friends. Would we have ever allowed this to happen? I even argued with people the term “concentration camp” was inflammatory and not helpful. When I saw the court recording, the pictures, and heard statements of lawyers I was shocked.
How could healthcare people not speak out? I hope that some of this information is getting out because they are leaking it. Yet, I don’t want to be too quick to forget what it is like to be the nurse in the facility. Each day you go in and see as many people as you can thinking if you aren’t there who will be there to provide the care. You go home and you pray for your patients. Yet the most obvious thing to do is sometimes the hardest. How do stand up to those in charge and say, not on my watch?
I’m outraged, but my outrage doesn’t change the current situation. CDR Jonathan White testified before the Energy and Commerce Committee on February 7, 2019. In his verbal responses, he was clear that people were warned about separating children and parents. He did not address all of the unaccompanied children that cross the border, but I’m sure he was equally concerned about them. Then in April 2019 before the Senate Homeland Security and Governmental Affairs, there was further testimony from CDR White and others. He appears to care about the welfare of the children and is trying to reunify children that came with parents or family member. In fact, for over a year ago HHS officials have warned about the situation. CDR White clearly states that the problem isn’t of data exchange, but that children were separated. The ORR program was designed for the truly unaccompanied children and not for children separated by the U.S. when apprehended. You can see the disgust on CDR White’s face when he says the issue is that it happened at all. Since July 2018 HHS has been warning the administration and Congress yet there is no positive action.
The Catholic tradition teaches that human dignity can be protected and a healthy community can be achieved only if human rights are protected and responsibilities are met. Therefore, every person has a fundamental right to life and a right to those things required for human decency. Corresponding to these rights are duties and responsibilities–to one another, to our families, and to the larger society.
My question to all of those screaming about the atrocities is what have you actually done to change it? Have you actually written a letter to your representative? Have you donated money to one of the not-for-profits that provide the care at most of the facilities for unaccompanied minors? And to Congress, other than the horrific legislation offered by Senator Graham that ignores the dangers faced by the asylum seekers, Senator Cruz’s Protect Children and Families Through the Rule of Law Act which is more about removal quickly back to the danger they fled, and U.S. Senator John Cornyn (R-TX) and U.S. Representative Henry Cuellar (D-TX-28) who proposed the HUMANE Act has anyone drafted legislation that would actually address the problems in the “concentration camps”? Is there anyone in the House or Senate that is working together to fix laws that allow this to continue?
If you really think this is inhuman, a concentration camp, and must be stopped then why not work day and night to pass legislation that will stop it? Isn’t that more productive that tweeting? I want to see a Tweet with a link to the legislative fix. I want to see posts about people volunteering with their local churches and community organizations to help support the needs of refugee families. In our parish, it took the hard work of five families to get one family to self-sufficiency. More volunteers are needed in almost every city in the country.
As for the rest of us, here is an interesting fact, anyone in the U.S., any citizen can draft legislation and a member of Congress can introduce it. I will write it if AOC will promise to introduce the legislation. I bet she even has some aides that could help. Likewise, what about all those running for President, where is your draft legislation to fix this?
We don’t need more hypocrisy. We need action that recognizes that our Puritan history must be weeded from our hearts, laws, and policies.
For I was hungry, and you gave me to eat; I was thirsty, and you gave me to drink; I was a stranger, and you took me in. (Matthew 25:35)
Like this:
Like Loading...